Six guiding principles for healthy, people-oriented change in healthcare
The contrast between innovative eHealth experiments and daily reality in healthcare couldn’t be any bigger. The tools and solutions used in practice do not improve the employee and patient experience, sometimes they even make things worse. How can this problem be solved?

Of course there are some amazing things that can be done in healthcare with technologies like augmented reality and artificial intelligence. But these amazing things do not feature in the daily reality of employees and patients. Their reality consists of tools designed with a focus on the technology and not on the people using it. If you think good design is expensive, you should see how much bad design costs. A complex, user-unfriendly interface can mean the difference between life and death in healthcare. The key to innovation lies in changing human behaviour and UX designers specialise in that. What can we add? From my expertise I have drawn up six guiding principles for healthy, people-oriented change in healthcare:
1. Empathy
We humans are 90 percent emotion and only 10 percent rational thought. Almost everything we do is done on the basis of feelings. The fact that a piece of technology does what it is supposed to do, does not automatically mean people will embrace it.
An example: the NHS in the UK had the idea to unburden GPs with a chatbot. Based on the answers to a number of questions, the chatbot could determine whether an appointment with the family doctor was truly necessary. An interesting idea, but the pilot was stopped prematurely, because it became clear that patients had found out how to answer the questions so that they would be sure to get an appointment with the GP. The need for human contact was simply not met by the chatbot.
Innovation does not have to be high-tech at all. A well-known problem is that stressed patients forget which questions they wanted to ask during the consultation with the doctor. You might think that this problem can be solved with an app. In one particular hospital they introduced paper coffee cups with 'Three great questions to ask your doctor.' A simple, cheap solution that is probably more effective than an app.
2. Ethics
In healthcare, clearly, security should come first. There’s a thermometer on the market in America which is ‘connected’. It raises the question of who actually owns the data that the thermometer collects. In this case, the data is sold on to advertisers of flu tablets. Of course they are very happy to know the regions where people’s temperatures are elevated, because they can then focus their online advertising campaigns there.
Privacy is important and not just for patients. A Dutch paediatrician told me that the national children’s healthcare centres, which monitor children’s development, are moving from closed electronic patient files to an open system that parents/caretakers can also consult. This has its benefits, as it creates engagement. But it also has a major drawback: the doctor no longer has the option to make personal notes. He or she can’t put a suspicion of abuse in the system if the parents are reading along. So what should the doctor do? Not write it down, with the risk of forgetting? Have a different system to note these kinds of things? It is important that these kinds of things are taking into consideration from the start.
3. Each other
We all talk about putting the user or patient first. But what does that actually mean? A doctor will always say that he or she puts the patient first, but the patient often does not feel that way. What we should focus on is relationships: relationships between the doctor and the patient, the patient and his or her family, and so on. If we design something, it should benefit both the sender and the receiver, otherwise it will never be a success.
A great example of this is the startup Fello, which is intended for family caregivers. It’s a shared calendar that allows people to take care of a family member together. It has been designed around the whole family, rather than the individual user. The app makes it much easier for the family to arrange who will take care of their family member when.
4. Elimination
The proverb 'prevention is better than cure' also applies to innovation. The best experience is no experience. At the moment we are doing research for a Dutch pharmacy chain on how we can prevent people from having to wait.
The use case for this is repeat medication. The current flow is: my pills have run out, I have to call the doctor for a repeat prescription. I don't know exactly when the medication will be available, so I call the pharmacy to check. Then I go to the pharmacy. Of course I have to take into account the opening hours and after arriving there I may have to wait in line.
That's how it has gone for years, but it doesn’t have to be this way. If I have an app that knows I'm using certain medication, it can remind me that it's time to order a new supply. The necessary information is already in the app, I can place my order at the push of a button. Then I have the choice: have it delivered, pick it up from a pharmacy employee or from a locker that can be opened 24 hours a day with the app
What matters is that we offer choices and that the new option is more attractive to specific user groups than the old one. At this particular pharmacy chain, the lockers already exist but the company hasn't gotten around to doing anything with them yet. The app exists but nobody uses it because nobody knows about it. So often it's about looking at what's already there and making sure those things are connected in the right way.
5. Embraceable change
People find it difficult to change. But if that change is advantageous to them, then they will embrace it. I read an interesting story on a blog recently about a nursing home where they switched from pagers to PDAs and where the call lights above the room doors were removed. From one day to the next. But the actual nurses and carers had never been consulted, with the result that the PDAs kept beeping but nobody knew who was where and people could no longer do their work.
This is because most eHealth applications are made by people who have never seen a patient. It’s an issue with an easy fix. If you think it's too early to test, then you should test. It's about constantly learning, as early and as often as possible to infinity. Start the project at the end. What do we want to say in a year's time when the innovation has been implemented? What is that one sentence that says what the value for the end user actually is? If you can't think of it in your first week, then the idea is too vague and you might be better off focusing your energy on something else.
6. Empowerment
Healthcare is about attention from and for people. But the reality is that doctors and nurses spend almost half of their time on administration, and this administrative pressure takes all the joy out of their work.
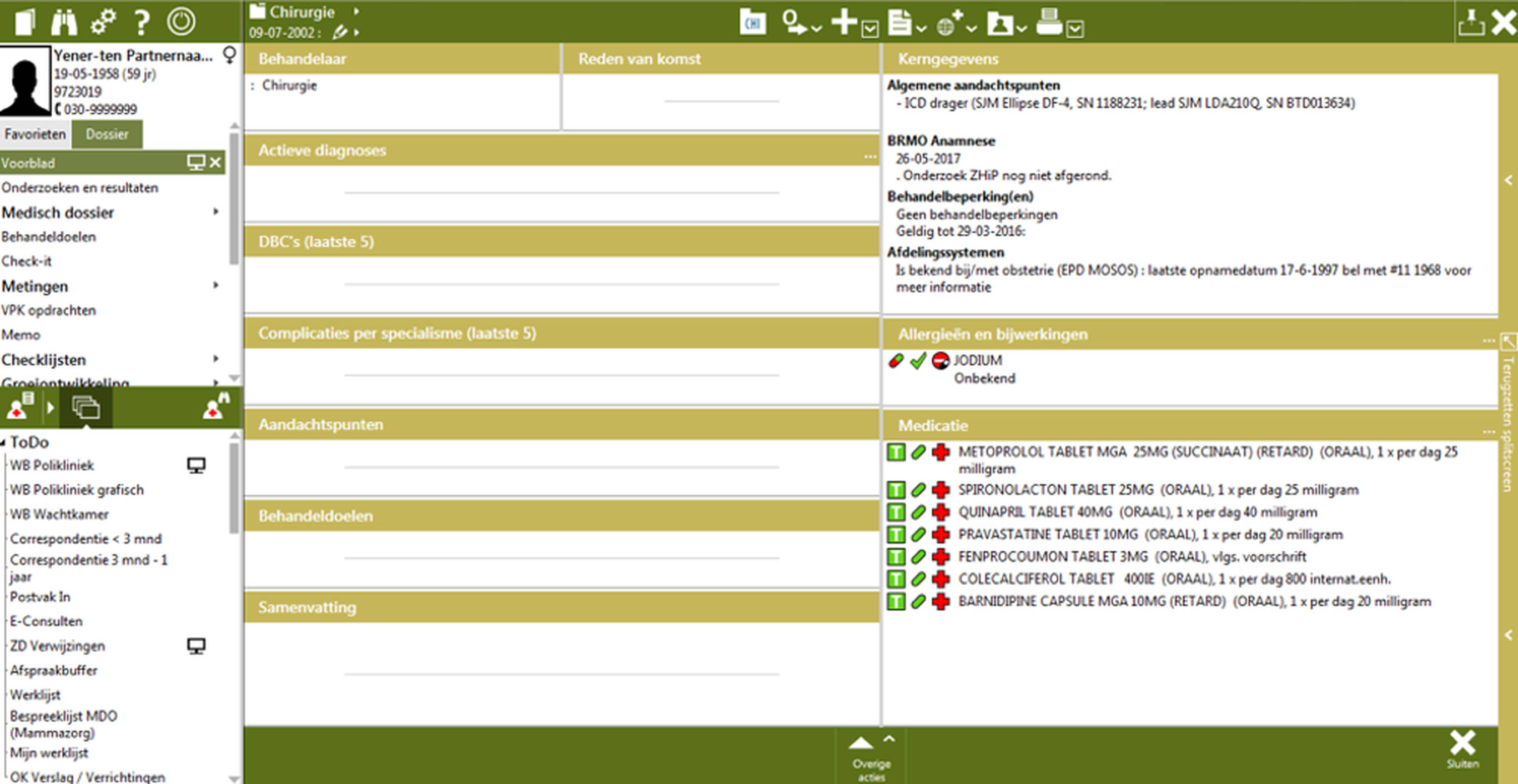
Administrative processes can be automated with tools that are meant to empower. Stethoscopes give doctors superpowers. They are intuitive and lightweight. But when it comes to digital tools, we come up with impossible user interfaces. Much of the frustration of healthcare workers is due to the fact that electronic patient files are not well designed.
The EPD before redesign:
The EPD after redesign:
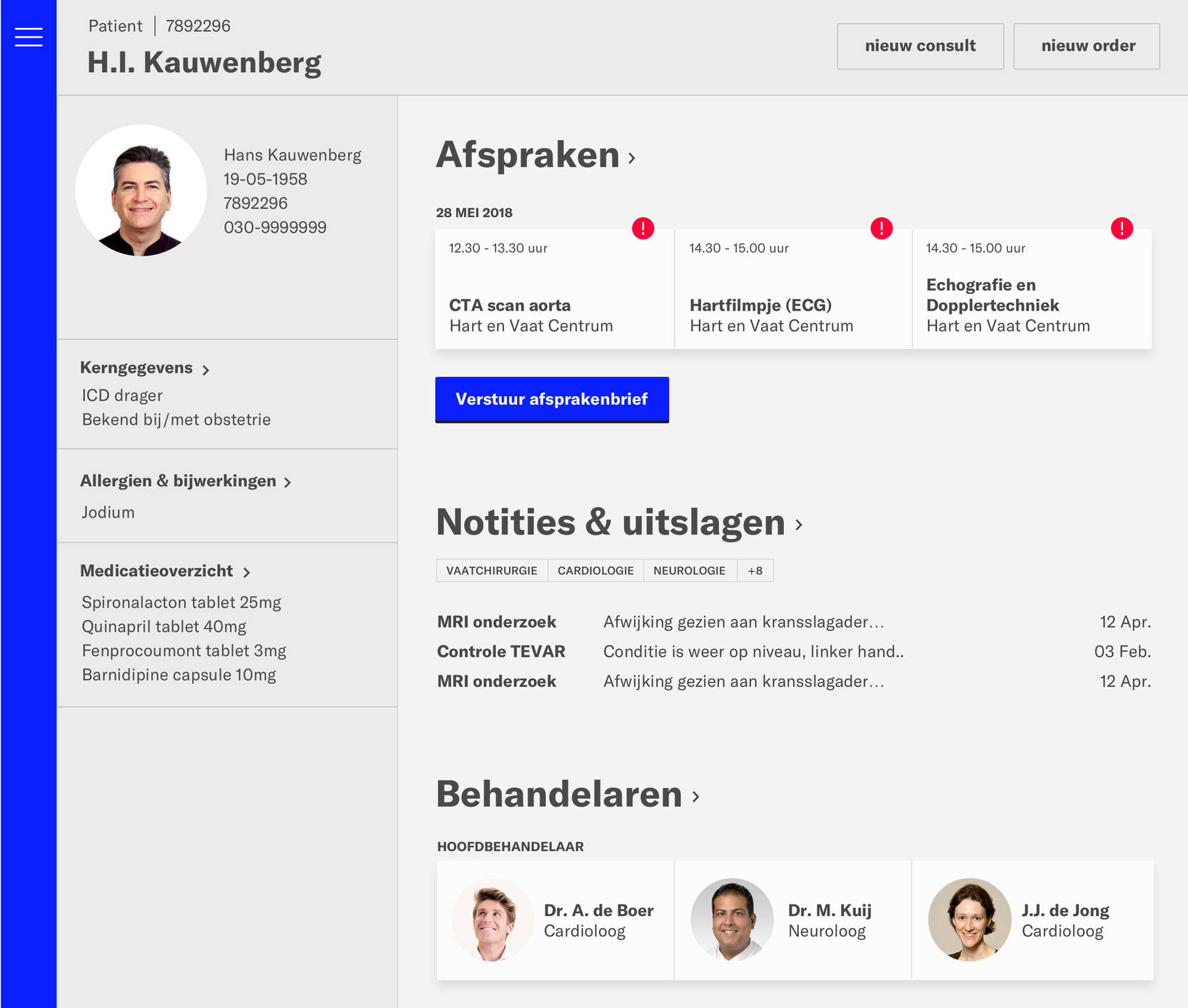
A number of my colleagues participated in a hackathon; in two days they translated an unreadable interface into a more useful concept. It might not yet be one hundred percent feasible or perfect, but the difference shows that there is room for improvement. We are already used to these kinds of intuitive interfaces in other sectors, such as retail and travel, but we have not yet reached this stage in healthcare. We will get there when we forget the technical e from eHealth and focus on one or more of the six new e's: empathy, ethics, each other, elimination, embraceable change and empowerment.